Pancreatic Cancer - Defying the Odds Eisenhower offers a new program for screening and prevention
In more than half of all cases, pancreatic cancer isn’t detected until stage 4, when it has already spread to other parts of the body. Less than 10 percent of patients survive five years past diagnosis, largely because the cancer shows few, if any, symptoms until it’s too late to intervene.
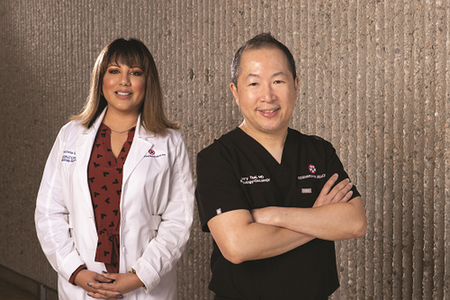
“The statistics are sobering,” says Henry Tsai, MD, Board Certified in Hematology and Medical Oncology, and Director of Gastroenterology Oncology at Eisenhower Lucy Curci Cancer Center. “Early detection is paramount to improving survival.”
Eisenhower Lucy Curci Cancer Center forged an affiliation in 2018 with UC San Diego Health, to benefit all Eisenhower cancer patients, bringing access to groundbreaking clinical trials, shared molecular tumor boards, a blood and bone marrow transplant clinic and a personalized immunotherapy clinic.
And new to Eisenhower, a cutting-edge pancreatic cancer prevention and screening program, in addition to one-on-one genetic counseling. This is welcome news for people at higher risk for developing pancreatic cancer due to family history, genetic mutations or other indicators like chronic pancreatitis (inflammation that doesn’t heal or improve).
Step 1: Find the Cancer
With screening for pancreatic cancer still in its early stages, widespread testing for the general population isn’t practical, “But we can focus on those at high risk,” notes Andrew M. Lowy, MD, FACS, Surgical Oncologist and Clinical Director for Cancer Surgery at Moores Cancer Center at UC San Diego Health. “Very early detection is transformative.”
Survival is improving for patients with pancreatic cancer identified at Stage 1A or even pre-cancerous - up from 45 percent to 84 percent. “Our goal is to catch the disease early in more and more patients or even prevent it,” says Dr. Tsai.
Initial imaging tests are performed at Eisenhower Lucy Curci Cancer Center, primarily magnetic resonance imaging (MRI) and endoscopic ultrasound, in which a thin tube and small, sound-wave emitting probe are sent to the abdomen to take a close-up look at the pancreas.
Patients are then evaluated by the team at UC San Diego Health. Individuals who don’t need immediate intervention are put on a regular schedule of monitoring. “It’s like I have someone watching out for me,” says screening patient Deborah DeSantis.
DeSantis, an Eisenhower employee, knew her extended family had a long history of cancer. Her mother died of ovarian cancer, her father of renal cancer and one of her grandfathers of pancreatic cancer, among others touched by the disease.
When her sister was diagnosed with breast cancer several years ago, tests showed no sign of the BRCA1 or BRCA2 gene mutations, most commonly associated with breast cancer. Then another of DeSantis’s relatives had genetic testing, which revealed the PALB2 gene mutation, a lesser-known mutation that increases the risk of breast, ovarian and pancreatic cancer.
DeSantis decided to have the genetic test as well and soon found she also has the PALB2 mutation. Last year, she enrolled in the pancreatic cancer prevention and screening program, which debuted at Eisenhower Health in November 2020.
Genetic Clues
“I had never thought about the genetic link with pancreatic cancer,” says DeSantis, who sees screening as a way to stay educated about her body. “Some people feel ignorance is bliss, but not me,” she adds. “I want to know. I’ve always been proactive about my health.”
DeSantis met with genetics counselor Diana DeRosa, MS, CGC, of UC San Diego Health, to discuss what they want to do. So far, some of her family members have been tested and also have the mutation.
As part of the screening program, DeSantis underwent an MRI at Eisenhower Health. It showed a small cyst on her pancreas - which doctors have opted to monitor for now.
Helping to coordinate DeSantis’s care, and that of other patients in the program, is Oncology Nurse Navigator Patricia Garcia, BSN, RN, CCRC, OCN, Eisenhower Lucy Curci Cancer Center. She serves as an initial point of contact and more. “I circle back with each patient to see if they need any follow-up testing, genetic counseling, nutritional guidance or other resources,” says Garcia. “I’m here to remove any barriers to patient care.”
Surgery remains the only treatment for pancreatic cancer, and it’s challenging. “You want a surgeon who is extremely experienced in this cancer,” says Dr. Tsai. Fortunately, Dr. Lowy is recognized worldwide for his expertise in pancreatic cancer surgery and complex gastrointestinal cancers.
Changing the Future
Another advantage for patients is a growing slate of research projects. Garcia told DeSantis about the PRECEDE Clinical Trial, offered by the Pancreatic Cancer Early Detection Consortium. UC San Diego Health is among the consortium members who seek to increase survival from pancreatic cancer to 50 percent over the next decade.
DeSantis enrolled. “I think about some of my family members who have passed away from cancer. Would knowing our shared genetic history have changed the course of their lives?” she says. “With this trial, I can potentially help future generations.”
For more information or to contact Eisenhower Lucy Curci Cancer Center, call 760.674.3602 or visit EisenhowerHealth.org/Cancer.