Still Feeling Fantastic

But what about longer-term outcomes? Do the benefits of spinal surgery last over time? For Palm Desert resident Inger Yarijian, 72, the answer is a resounding “yes.”
Yarijian had had a “bad back” since she was a teenager growing up in her native Norway. By the time she was in her late fifties, living in California and working as a pre-testing assistant in an ophthalmologist’s office, the pain was severely compromising her ability to live and work.
“It got to a point that everything was difficult to do,” she says. “Walking too much, standing too long, sitting too long…it wasn’t good. I’d have to lie down to rest and even turning over in bed was excruciating. Sometimes I’d decide to go shopping, park as close to the store entrance as possible, but end up turning around and going home because the pain was so bad.
“I knew I had to do something,” she continues. “Then I saw an article in Healthy Living magazine about Dr. Shen and decided I had to go see him.”
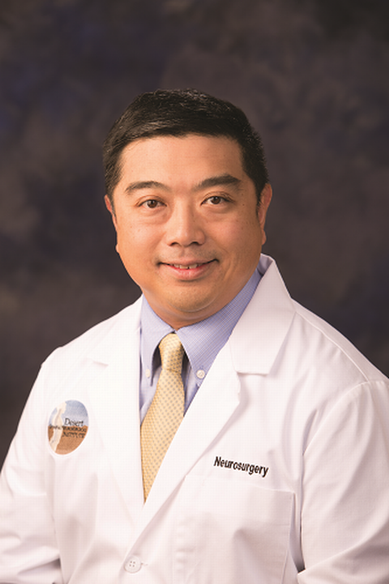
“I began seeing Mrs. Yarijian for her back pain in 2006,” recalls Alfred Shen, MD, who is Board Certified in Neurological Surgery. “Her workup revealed that she had degenerative disc disease at the L5/S1 spinal motion segment.” Also called the lumbosacral joint, this is the area between the lumbar spine and sacral spine in the lower back that helps transfer loads from the spine into the pelvis and legs.
“She also had spondylolysis, or what’s called a pars defect,” he notes.
“Typically, a pars defect starts out as a little crack, but as you continue to do certain activities, it never heals and starts to loosen,” he continues. “With her life activities, Mrs. Yarijian did a lot of bending and twisting, which aggravated it, causing the symptoms she was experiencing.
“For about three years, we tried standard conservative treatments including physical therapy, epidural steroid injections, acupuncture, anti-inflammatory medications and a corset, or back brace,” Dr. Shen continues. “These conservative modalities would provide temporary relief. But the pain got progressively worse, extending down her right leg. It was time to consider surgery.”
Yarijian underwent surgery in April 2009. Dr. Shen performed a laminectomy at L5 (the fifth lumbar vertebra), a decompression procedure in which the back of the vertebra is removed to relieve pressure on nerves. He also performed a discectomy (surgical removal of an intervertebral disc) and interbody fusion with instrumentation at L5-S1. This allowed for stabilization between the L5 and S1 vertebral bodies as well as releasing pressure on the traversing nerve roots.
“We paid particular attention to the L5 nerve root and made sure it was well-decompressed,” he notes.
Yarijian spent three days in the hospital. “I recall feeling pain-free right away after surgery,” she says. “But it took a few months before I went back to work. Being able to walk again — and simply stand — was the best!”
In the 12 years since her procedure, she says her back as been “fantastic.”
“I know I can’t overdo things, so I’ve learned to be careful and follow Dr. Shen’s advice,” she adds. “But when you feel good, sometimes you start doing things you shouldn’t do.”
Case in point: she saw Dr. Shen this past July when she suddenly started experiencing back and neck pain.
“I initially thought she might have a problem at another level of her spine, but imaging showed that all her other discs looked fine, including the adjacent level to her prior fusion,” he relates. “Turns out, she had overreached when she’d stooped to pick up a watermelon, spraining her back. We treated her conservatively and everything resolved.
“Since completing surgery more than a decade ago, Mrs. Yarijian has been mindful of her posture and body mechanics — except for the watermelon — which has definitely helped with her good long-term outcome,” he adds. “If I saw her for the first time today with the same symptoms that she presented with in 2009, I would again treat her conservatively before recommending the same operation.”
“And I would have it,” says Yarijian. “Dr. Shen saved me.”
To learn more about Eisenhower Neuroscience Institute, call 760.837.8020 or visit EisenhowerHealth.org/Neuro