Revolutionizing Cardiac Care: Leadless pacemakers offer renewed hope and vitality
Although pacemakers have undergone significant advancements through the decades, next-generation leadless pacemakers have emerged as a game-changing option for treatment and increased quality of life.
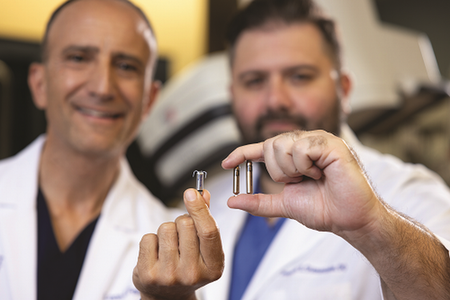
At Eisenhower, Board Certified Cardiologists Evangelos Diamantakos, DO, and Leon Feldman, MD, are leading the way in implementing this new technology. Dr. Feldman was the first cardiologist in Southern California to implant Medtronic’s Micra™ AV2 and has completed more than 300 procedures with the Micra ™AV1 and AV2 devices. In the fall of 2022, Dr. Diamantakos performed the first Abbott Aveir™ VR leadless pacemaker implant in Riverside County.
“The evolution from transvenous pacing systems to leadless platforms is a major advantage for patients at high risk for complications,” says Dr. Diamantakos.
“The leadless pacemaker has an exceptionally low risk of infection,” says Dr. Feldman. “In fact, if a patient has a pocket- or lead-related infection from a conventional pacemaker, we can simultaneously and safely retrieve the implanted pacemaker and replace it with a leadless device.”
Wireless wonders
The Micra and Aveir pacemakers are less than one-tenth the size of traditional pacemakers — smaller than a AAA battery. The enhanced devices offer a battery lifespan averaging anywhere from 15 to 20 years, meaning that patients will likely only need one device for life.
Unlike traditional pacemakers which require surgically inserting a generator pocket under the skin below the collarbone with tiny wires called leads that connect to the heart, leadless devices eliminate the need for a chest incision so there is no visible scarring or bumps. The minimally invasive procedure takes 30 minutes to an hour, using a transcatheter delivery system via the right femoral vein to guide and position the tiny pacemaker into the right ventricle.
“The tip of the Aveir leadless device provides us with real-time electrical mapping of the tissue, reducing the need to reposition,” explains Dr. Diamantakos. “This live feedback helps us determine the optimal area to implant the pacemaker.”

“Our standard practice is to check the pacemaker implant a day after the procedure to ensure that patients are safe to go home and the pacemaker is functioning properly,” he continues. “The fidelity, stability and electrical characteristics of these devices are so good that this extra step is becoming unnecessary.”
Individuals who may benefit from single chamber leadless pacemakers include those with atrial fibrillation (AFib), bradycardia, bradycardia-tachycardia syndrome, patients who require occasional pacing, and those with comorbid conditions like diabetes or renal disease.
Patients who have atrioventricular (AV) synchrony, or heart block, a condition resulting from a dysfunction of the electrical signals that travel through the upper chambers (atria) to the lower chambers of the heart (ventricles) may also be appropriate candidates. Both the Micra and Aveir
pacing systems are equipped with sensing algorithms to coordinated pacing between the atrium and ventricles.
Leadless dual chamber technology
In July, Abbott marked a significant advancement in cardiac care, securing FDA approval for the AVEIR™ dual chamber (DR) leadless pacemaker. The pacing system consists of two small devices for the right ventricle and the right atrium. According to the company, more than 80 percent of people require pacing in two chambers of the heart — the right atrium and right ventricle. The system is also upgradeable so that treatment can be customized and adapted to patients’ needs, using one or both devices.
For heart patients dealing with arrhythmia-related heart failure and other cardiac conditions that require a biventricular pacemaker, Diamantakos is optimistic that science and innovation are forging ahead to develop that technology.
“I think in the future there will be a lot of dialogue around developing a completely leadless three-chamber system,” he adds. “But right now, it’s in the infancy stages of discussion.”
For more information or to contact Eisenhower Desert Cardiology Center, call 760.346.0642, or visit EisenhowerHealth.org/DesertCard.



